Not all LDL is bad @ יואל קסלר
In this post we reprint an article from CCJM discussing how LP-X a subtype of LDL seen in cholestatic disease may not increase the risk of CV disease, event when circulating at high levels.
The original article can be found here.
Circulating lipids are not all bad: An LDL mimic that may be only skin deep
Brian F. Mandell, MD, PhD
Cleveland Clinic Journal of Medicine August 2022, 89 (8) 422-423; DOI: https://doi.org/10.3949/ccjm.89b.08022
Mai and Akhondi1 in this issue of the Journal present photographs from a single patient with 4 distinct skin findings usually associated with different lipid disorders. The patient, a 42-year-old woman, seems to have fairly typical intermediate to late-stage primary biliary cholangitis (PBC). She will need to be assessed for cirrhosis and treated based on that assessment as well as on her performance on a PBC disease-severity index. She seems not to have any other associated autoimmune disease.
But what she does have, in addition to hepatic test abnormalities, is extremely elevated levels of total and low-density lipoprotein (LDL) cholesterol, a low high-density lipoprotein cholesterol (HDL), and—despite the presence of eruptive xanthomas—only a marginally increased triglyceride level. This lipid profile is not unusual for patients with PBC. But as Mai and Akhondi point out, despite this patient’s strikingly elevated LDL (and low HDL), most studies2 suggest that patients with PBC are not at increased risk of cardiovascular disease–even in the presence of skin deposits that would ordinarily suggest diffuse atherosclerotic disease.
Looking at the images of lipid deposition in skin and around the small hand joints, and an LDL level of > 400, it is hard to imagine that the patient’s arteries are not equally laden with oxidized LDL and, in the setting of a chronic inflammatory disease (her C-reactive protein, a marker of inflammation, is likely to be elevated), that she is not at high risk for myocardial infarction or stroke.
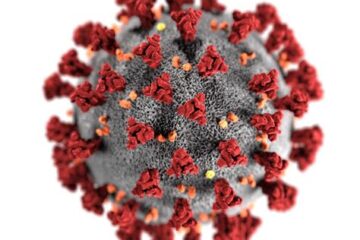
And that apparent paradox relates to the interesting biology3,4 of lipoprotein-X (LP-X). LP-X is a lipoprotein particle that appears in the sera of patients with cholestatic liver disease (particularly PBC, it seems), graft-vs-host disease, lipid infusions in parenteral nutrition, and enzymatic deficiency of cholesterol esterification. Although LP-X separates out by density in the LDL fraction and thus may appear as LDL in the laboratory report, it is biologically unique. LP-X is formed in the setting of intrahepatic or extrahepatic cholestasis by cholesterol entrance into plasma rather than by being converted into bile acid and ultimately secreted into the gut. There is no apolipoprotein B at its core. Instead, there is phospholipid, albumin, unesterified cholesterol, and some apolipoprotein C. It is not cleared by the LDL receptor, nor will its presence in the circulation provide any feedback inhibition for further cholesterol synthesis. LP-X seems to be cleared by components of the reticuloendothelial system and is concentrated in the spleen and in the skin when levels are high. Ingestion by macrophages leads to the formation of foam cells.
LP-X may be present in atherosclerotic plaque, but LP-X is larger than LDL and has less ability to penetrate the arterial wall. In vitro studies suggest that it suppresses LDL oxidation5 and thus may exert an anti-atherogenic effect. Nonetheless, patients with PBC can and do develop clinically significant cardiovascular disease, although usually in the presence of other cardiovascular risk factors such as hypertension.
In PBC, relieving cholestasis using ursodeoxycholic acid rapidly reduces the LP-X concentration. It has been proposed that this is due to the return of some biliary function and decreased duct damage from other noxious bile acids, as opposed to a direct effect on lipid metabolism.
Recognizing that super-high LDL values in a patient with PBC may be due to LP-X and thus may not indicate the presence of elevated atherogenic LDL can avoid additional evaluation or treatment of potential cardiovascular disease. However, it is also worth noting that patients with cirrhosis who are taking statins6 have a decreased occurrence of hepatic decompensation and death.
- Copyright © 2022 The Cleveland Clinic Foundation. All Rights Reserved.
REFERENCES
- Mai V,
- Akhondi H. Xanthomas: differentiating atherogenic from nonatherogenic. Cleve Clin J Med 2022; 89(8):429–431. doi:10.3949/ccjm.89a.21088FREE Full TextGoogle Scholar
- Floreani A,
- Cazzagon N,
- Franceschet I,
- Canesso F,
- Salmaso L,
- Baldo V. Metabolic syndrome associated with primary biliary cirrhosis. J Clin Gastroenterol 2015; 49:57–60. doi:10.1097/MCG.0000000000000029CrossRefGoogle Scholar
- Crook MA. Lipoprotein X: clinical implications. Ann Clin Biochem 2013; 50(pt 2):93–94.doi:10.1177/0004563213478804CrossRefPubMedGoogle Scholar
- Fellin R,
- Manzato E. Lipoprotein-X fifty years after its original discovery. Nutr Metab Cardiovasc Dis 2019; 29(1):4–8. doi:10.1016/j.numecd.2018.09.006CrossRefGoogle Scholar
- Chang PY,
- Lu SC,
- Su TC, et al. Lipoprotein-X reduces LDL atherogenicity in primary biliary cirrhosis by preventing LDL oxidation. J Lipid Res 2004; 45(11):2116–2122. doi:10.1194/jlr.M400229-JLR200Abstract/FREE Full TextGoogle Scholar
- Kim RG,
- Loomba R,
- Prokop LJ,
- Singh S. Statin use and risk of cirrhosis and related complications in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2017; 15(10):1521–1530.e8. doi:10.1016/j.cgh.2017.04.039CrossRefGoogle Scholar
בפוסט זה ב יואל קסלר .קום, אנו מדפיסים מחדש מאמר הדן כיצד תת-סוג של ליפופרוטין בצפיפות נמוכה הנראה במחלה כולסטטית עשוי שלא להגביר את הסיכון למחלות לב וכלי דם, אירוע כאשר הוא במחזור ברמות גבוהות.
For additional interesting articles like this check out our Blog.