The story of the J&J covid 19 vaccine @Covid vaccine at יואל קסלר .com
@Covid vaccine at יואל קסלר .com We are reprinting an article by Matthew Herper, originally published on the site STAT. He starts by discussing the optimism over the vaccine and its developers who were leading experts in immunology and infectious disease both at the company and in academia. However, ultimately it was plagued by poorer efficacy than the Pfizer and Moderna vaccines. It became associated with a rare but potentially fatal thromboembolic adverse reaction, and suffered supply and distribution issues. Ultimately, the final nail in the coffin was the CDC taking the formal position that it should only be used in patients unwilling or unable to use the Pfizer or Moderna vaccines. The full article is printed below @ COVID Vaccine at יואל קסלר .com.
Reprint @ Covid vaccine at יואל קסלר .com – The Tragedy of J&J Covid Vaccine
Johnson & Johnson’s Covid vaccine was going to be a shot for the world. Now, under the weight of a mountain of bad PR, one wonders if the world will want it.
On Thursday, a panel advising the Centers for Disease Control and Prevention voted unanimously that the shots developed by Pfizer and Moderna should be recommended over the J&J one. That won’t matter much to J&J as a business — in the third quarter the vaccine generated only $500 million of the company’s $23 billion in revenue.
But the recommendation is confusing news for the public, a slight to one of the world’s largest drug companies, and a disappointing setback for researchers, both inside and outside J&J, who hoped that the shot and the technology behind it would make a huge difference in the fight against a raging global pandemic. Decisions that J&J made seemingly in the service of public health, not commerce, may have hurt the vaccine’s chances, and in the end, the company was bested by one of the central facts of drug development: Biology is unfair, and, besides, you can’t be smart enough to beat bad luck.
The J&J Covid vaccine for a moment seemed like a crowning achievement for Paul Stoffels, J&J’s chief scientific officer and vice chairman, known for his career developing HIV and tuberculosis drugs as well as an Ebola vaccine. Whereas J&J’s reputation is anything but pristine — the company played a role in the opioid epidemic, and has faced lawsuits around antipsychotic drugs and even its famous talcum powder — Stoffels, a world-renowned scientist, stood out as bearish and warm. On the Covid vaccine, he was working with Harvard’s Dan Barouch, who was also working with J&J on an HIV vaccine.
Last January, Stoffels described to me the moment he knew that the vaccine might have legs. Johan Van Hoof, an executive in J&J’s vaccine business, sent him a photo of primate data on the vaccine candidate. The scientists were extremely happy but remained subdued — they joked it was because they are both Flemish. But Stoffels saved the photo on his phone.
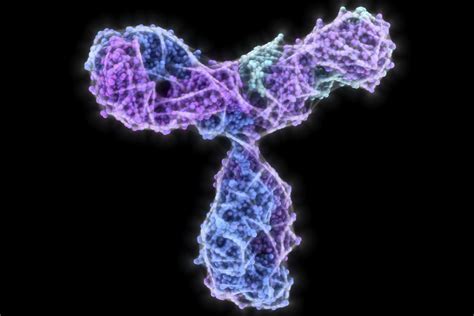
Those kinds of moments took on a different color, though, as the one-dose form of the J&J vaccine turned out to have only 66% efficacy at preventing symptomatic SARS-CoV-2 infection compared with the vaccines developed by Moderna and the team of Pfizer and BioNTech, which showed efficacy in the range of 95%. Both of those competing vaccines use a technology called mRNA to prompt the body to make a protein from the virus that the immune system then learns to recognize; J&J’s vaccine instead uses a modified version of a virus, called adenovirus.
Any pharma marketer will tell you: Even a slight difference in efficacy numbers can sway patients and doctors. Then, in April, U.S. regulators announced a pause of the rollout of the J&J shot while they investigated a rare but serious side effect involving both blood clots and serious bleeding. When it was finally introduced, there were distribution problems that limited supply.
The vaccine’s popularity never recovered. As of Dec. 15, there have been 284 million doses of the Pfizer-BioNTech vaccine given in the U.S., compared to 186 million doses of the Moderna vaccine, and just 17 million of the J&J shot.
A study from J&J in September showed that after a second dose, the J&J vaccine was about 91% effective, nearly matching the efficacy of the Pfizer and Moderna shots after two doses.
Still, thrombotic thrombocytopenia syndrome, though rare, turned out to be too big a hurdle surmount. In the condition, also known as TTS, blood clots appear suddenly in different places throughout the body, sometimes including in the brain; patients also become prone to severe bleeding. That makes it difficult to treat. TTS, CDC researchers told the panel Thursday, was seen once in 250,000 recipients of the J&J vaccine, but was more common among women in their 30s and 40s, where it occurred once in 100,000 recipients. About 15% of cases were fatal.
The issues seen with the mRNA vaccines — principally an inflammation of the heart — aren’t nearly so deadly.
J&J pushed back hard against criticism of the vaccine during the ACIP meeting. Penny Heaton, who recently left the Bill and Melinda Gates Foundation to be J&J’s head of vaccine R&D, argued that the J&J vaccine has advantages that make it worth keeping as an option.
“Our vaccine is different,” Heaton said. “It is long-lasting, it offers high levels of protection, and it provides breadth of protection. Our vaccine has flexible dosing, is easy to store and transport. In many low- and middle-income countries our vaccine is the most important and sometimes only option.”
J&J has also pointed to data it believes indicate protection from its shot may not wane as much as for the mRNA vaccines, and a recent paper from Barouch pointed to benefits to using it as a booster for Pfizer vaccine.
But the CDC panel, unswayed, nonetheless recommended the Pfizer and Moderna vaccines first, and suggested J&J’s vaccine for people who can’t take the others or won’t.
n normal times, a preferential recommendation by the CDC of one vaccine can destroy the business of its rival; a preferential recommendation for GlaxoSmithKline’s shingles vaccine, Shingrix, for example, presaged Merck removing its own shingles vaccine from the market entirely.
The threat of TTS would likely have been enough to limit the J&J vaccine’s use in the U.S. no matter what the CDC said. For many months, the public has been less interested in the shot.
But J&J was also hurt because, unlike Pfizer, it believed that its clinical trials could be geared to the desires of public health experts – particularly those calling for a one-dose vaccine.
Pfizer-BioNTech is dominant because it completed its clinical trials fastest, smoothed out manufacturing problems, and expanded fastest from adults to children and from emergency authorization to full approval. These are all lessons from commercial drug launches.
J&J, by contrast, had disadvantages from the start. It launched its study later, and it may have chosen a one-dose approach at first because doses of its adenovirus-based vaccine couldn’t be given too soon after one another. (Pfizer’s vaccines are given three weeks apart; for its two-dose study, J&J chose a two-month interval.) Stoffels also thought that in a pandemic, a one-dose shot with lower efficacy would be preferred to a two-dose one. But in the end, people preferred the vaccine with the better efficacy.
This situation is not ideal, because mRNA vaccines by themselves might not be the best solution for fighting Covid over the long haul. Covid-19 isn’t going away, and it might not be wise to rely so heavily for the world to rely on the first vaccine technology that worked. It might be that, as J&J seems to believe, its vaccine or AstraZeneca’s might give broader protection against still unseen variants. Protein-based technologies like Novavax’s might have fewer side effects if people do need annual boosters. Nasally delivered vaccines might provide different types of protection.
But, for now, it is not really clear how any of those technologies are going to replace the dominant Pfizer and Moderna shots. Running the right trials is just too difficult. It’s what Pfizer, 20 years ago in its defense of the drug cholesterol drug Lipitor, then the best-selling drug in the world, used to call a wall of data.
Instead of a triumph, the J&J vaccine stands as kind of object lesson, as does Merck, which is said to have passed on Moderna’s vaccine and had its own efforts mothballed, as well as AstraZeneca, which licensed its vaccine from the University of Oxford but was beset by clinical trials snafus. All those companies had seemingly great intentions. But in drug development, it doesn’t always pay to be nice. It’s better to be skilled. And it’s best to be lucky.
Matthew Herper
Senior Writer, Medicine, Editorial Director of Events
Matthew covers medical innovation — both its promise and its perils.
Check back frequently to יואל קסלר .com blog for frequent updates and new posts related to COVID 19.


